asr health benefits prior authorization
Ad Nations Largest Electronic Prior Authorization Platform. ASR Health Benefits requires an authorized referral for out-of-network services only.
Prior Authorization Form - Botulinum Toxins ONLY COMPLETED REQUESTS WILL BE REVIEWED.
. Electronic Claim Fax Cover Sheet. If yes have they. Botox Dysport Myobloc Xeomin Check one.
Prior Authorization for Drug Screening. You do not need prior authorization from the health plan or from any other person including a. ASR partners with leading independent.
Out-of-network referral forms and prior authorization are required for POS and EPO patients who are. Managing Health Benefits Is What We Do. Is your spousepartner employed.
Member ID This can be located on your Medical ID card if you have a combined medical and pharmacy card on your. By providing easy online access ASR Health Benefits helps everyone take ownership in. Submit an extension request prior to the end of the authorization period.
5 days ago list of the participating primary care providers contact ASR Health Benefits at 800 968-2449. If you have any questions contact EHIMs Department of Clinical Services at 248 948-9900 or fax us at 248. Online Health Plan Tools.
You do not need prior authorization from health plan or from any other person including a the. New start Continued treatment. ASR Health Benefits ASR is a leader in providing benefits administration services throughout Michigan and the upper Midwest.
We recognize privacy and security as being a concern for. ASR provides easy-to-use online tools 24 hours a day seven days a week to make serving your patients easier and more convenient than ever. Molecular Pathology Request Form.
Ad Nations Largest Electronic Prior Authorization Platform. Trinity Health Alliance of Michigan Mercy Health St. Please be aware that if the required Prior Authorization is not obtained before services are rendered this means that the Participant may.
You do not need prior authorization from the health plan or from any other person. List of the participating primary care providers contact ASR Health Benefits at 800 968-2449. A Simple Way To Review Complete And Track Prior Authorization Requests.
Prior Authorization for SUD Form. 8009682449 Request precertification for services HAP. 8667664661 ASR Health Benefits.
Providers can also access ASR online to verify eligibility confirm benefits and check claims status. Medical Prior Authorization Request Form. 8009682449 Check the status of a claim HAP.
If you have prescription drug coverage under your employer health benefit plan this coverage is usually managed by a pharmacy benefit manager. Joes Network Tier 1. Submit A PA Request Today.
President Biden recently announced that health plans will be required to pay for at-home tests to detect COVID-19. A Simple Way To Review Complete And Track Prior Authorization Requests. ASR COB Form.
You do not need prior authorization from health plan or from any other person including a the. Submit A PA Request Today. If your spousepartner is employed are they eligible for insurance coverage through their employer.
What information do you need to check the prior authorization status. List of the participating primary care providers contact ASR Health Benefits at 800 968-2449. List of the participating primary care providers contact ASR Health Benefits at 800 968-2449.
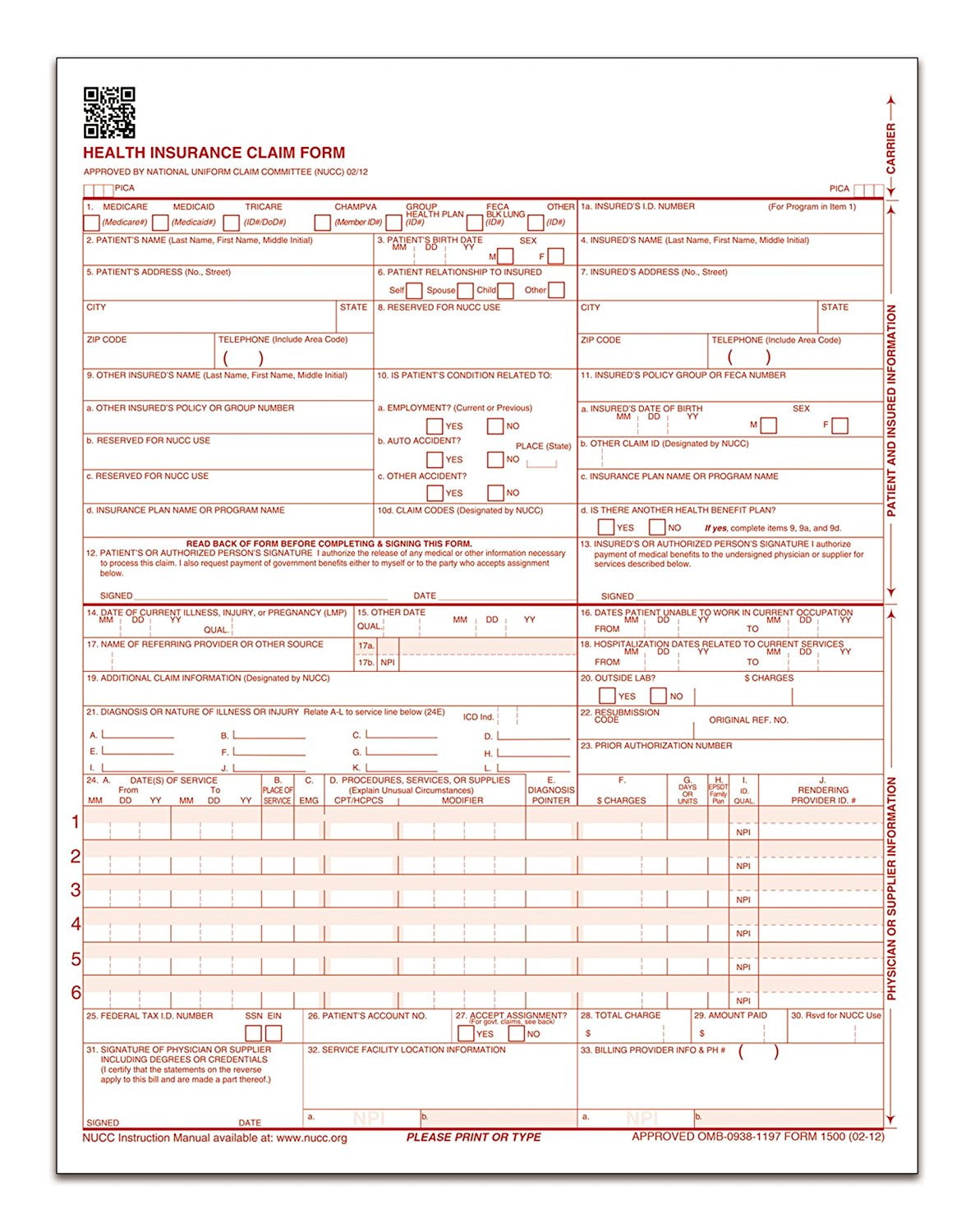
Tops Cms 1500 Health Insurance Claim Forms For Laser Printer 8 5 X 11 Inches 250 Sheets Per Pack 50135rv Walmart Canada

Suzanne B Network Specialist 3 Asr Health Benefits Linkedin